As we enter 2021, we are filled with hope that the vaccines developed in 2020 will alleviate the suffering of worst global pandemic in over one hundred years. There has been much said about the rapid development, testing, and approval of the vaccines to prevent the spread of Covid-19. However, much of the speed involved is the result of many years of accumulated research and almost instant access to the huge amount of capital resources needed to get the job done. Multiple, large pharmaceutical companies backed by government guarantees to purchase the new vaccines as soon as they have been tested and approved has all but assured the world community that help would arrive faster than ever before.
However, the speed and success seen over the past few months wasn’t the case a hundred years ago. Government entities and the scientific community didn’t always work in unison. Large pharmaceutical companies were more interested in purchasing the rights to medicines that had already been patented and made ready to market than they were in funding the research and testing that was needed to produce them. What can be accomplished in months today, required years back then.
Polio, or Poliomyelitis, is a crippling communicable disease caused by a virus. There are three types of poliovirus and many strains of each type. The virus enters through the mouth and multiplies in the throat and gastrointestinal tract. It then moves into the bloodstream spreading throughout the central nervous system where it replicates and destroys the motor neuron cells. Motor neurons control the muscles for swallowing, circulation, respiration, as well as the movement of the arms, and legs. There is no cure.
Since the virus is easily transmitted, epidemics were commonplace in the first decades of the 20th century. The first major polio epidemic in the United States occurred in Vermont during the summer of 1894. By the second decade of the 20th century thousands were affected every year. Early treatments were extremely limited. Government mandated quarantines were imposed upon houses, sometimes even entire streets, where victims lived. Beginning in 1916, polio epidemics appeared each summer in various parts of the country, with the most serious outbreaks occurring in the 1940s and 1950s.
Unlike the Corona virus we are battling now, polio was more severe among the youngest members of society. In the United States, the annual incidence of poliomyelitis reached epidemic proportions during several years in the 1930’s and 1940’s, resulting more than 10,000 cases of at least partial paralysis each year. Recovery was slow and often incomplete. In nearly half of those cases, the muscle weakness subsided in less than a year and was not the cause of a permanent disability. But just like today’s Corona virus, the ability to breathe on one’s own during those critical months was a major concern, and without some form of mechanical assistance it could often lead to death.

As a result of this need, in 1927, the iron lung, a negative pressure ventilating machine was invented to address the needs for assisted breathing during the recuperation from polio. The large apparatus enabled patients with polio to breathe on their own. Most patients spent weeks or months in the iron lung to reverse the paralysis of chest muscles.
At the height of the polio outbreaks, rows of iron lungs filled hospital wards to help patients with paralyzed chest muscles breathe. Many patients were able to leave the hospital, but only when one of these machines was made available for them at home. In 1939, the cost of one of these apparatuses was around $1,500 – or about the same price as a new automobile. Many of these were paid for by charitable organizations such as the March of Dimes or local chapters of fraternal clubs such as the Lion’s International.


Today, modern mechanical ventilators, employing positive pressure ventilation systems, are the standard of care. They work by blowing air into the lungs, whereas the iron lungs popular in the 1930’s, 40’s and ‘50’s used a vacuum to create negative pressure within the machine that allowed the patient’s lungs to expand and capture oxygen on their own.
During the larger annual outbreaks of poliomyelitis, as many as 5,000 young victims required prolonged, or even permanent, assistance to return to daily life. Heavy iron braces worn on the legs, along with specially designed metal canes or crutches were needed for mobility. These often weighed as much as fifteen pounds and sometimes required additional assistance when being fitted for daily wear by the user. While many patients eventually regained enough muscle strength to shed these devices, far too many did not. Some victims of the disease would require their use on a permanent basis.

Returning to school was especially difficult for some of these children. Not all school administrators were welcoming and there were almost no provisions in those days to accommodate handicapped students in any way. From Richard J. Altenbaugh’s The Last Children’s Plague, Chapter Six, The Cripples:
Through the first half of the twentieth century, school administrators responded in a variety of ways to students affected by infantile paralysis who wanted to return to school. In the 1940s, as physicians at the Orthopedic Clinic of New Haven Hospital discharged patients, hospital personnel sent letters to their school principal or school nurse, designating part-time or full-time attendance as well as excusing them from physical education class. However, some schools refused to even readmit them. Following six-year-old Clara Yelder’s treatment at Tuskegee’s Infantile Paralysis Center, the local public school superintendent refused to re-enroll her, thereby ending her formal educational experience. Robert C. Huse felt completely unwelcome: “When I applied for admittance to high school the principal had said he was doubtful it would work . . . It was obvious he did not want the responsibility of my being there.” If readmitted, generally speaking, the only building preparations administrators made consisted of relocating all classes to the first floor. Michael W. R. Davis found his neighborhood Louisville school to be completely unresponsive. He had to continue his daily hot pack treatments every morning at home and needed to continue to visit the hospital’s physical therapist. His school’s principal proved too inflexible to alter the daily schedule in any way for him. His parents instead had to enroll him in a local private school that accommodated his fragmented attendance. By October, the morning hot pack treatments stopped, and he was able to attend a half-day for five days a week. His treatments became less frequent by January, allowing him to attend school on a full-time basis… Siblings occasionally paid a price. Shelby Sigmon, age four, contracted poliomyelitis during North Carolina’s 1944–45 epidemic. Her sixteen-year-old sister, Clara, visited her daily at the Hickory emergency treatment center. Clara’s high school principal, fearful of her being a possible carrier, ordered her to his office and gave her an ultimatum: stop visiting her younger sister or quit school. Clara chose her sister over her formal education.
The first serious attempts to produce a vaccine for the prevention of Poliomyelitis came in the early 1930’s. In spite of its relatively low impact in terms of overall mortality and morbidity, polio was seen as an especially threatening disease because it mainly killed or crippled children; it had no obvious relation to poverty; and there was seemingly no way of preventing either its onset or its spread. Two American scientists, Maurice Brodie from the public health laboratory of the city of New York, and John Kolmer, working for the Institute for Cutaneous Medicine in Philadelphia, began clinical research on separate vaccines. That research was followed by limited trials on animals and then more extensive trials on human children.
Both Brodie’s and Kolmer’s vaccines were less than perfect. Kolmer’s vaccine, produced from live strains of the virus, was found to produce the disease where there had been no other exposure to it other than the vaccination. Kolmer’s efforts resulted in the death of several subjects from the polio contracted from his vaccine, while many more were paralyzed, made ill, or suffered severe allergic reactions. Brodie’s vaccine, while more promising, did not produce a sufficient level of protective antibodies to protect a large enough percentage of those participating in the clinical trials. It also produced severe allergic reactions in several of his test subjects. It was soon concluded that neither man had conducted extensive enough tests on animals before turning to human experimentation. In the 1930s, experimentation on human beings was not regulated by the law, and the accidents of anti-polio vaccination were mostly hidden from the media. Nevertheless, the discovery of the existence of such accidents by Kolmer’s peers led to a rapid interruption of his vaccination campaign. Kolmer’s abject failure ultimately led to New York abandoning Brodie’s trials as well for fears that similar tragedies might occur in other children.
In 1937, an antibiotic sulfa drug manufactured and sold by the S.E. Massengill Company killed 100 people. The drug contained an untested solvent known as diethylene glycol – a substance used in automotive brake fluid and antifreeze. As a result of this tragedy, Congress passed the Food, Drug and Cosmetic Act of 1938. The new law greatly expanded the regulatory powers of the Food and Drug Administration, requiring a full review of all new pharmaceutical products prior to the agency granting approval for sale and distribution. The new powers granted to the FDA made the development and test trials of vaccines almost prohibitively expensive and put many of them on the back burner. When the United States entered WWII, almost all funding for scientific development of vaccines was diverted to the war effort.
For well over a decade, the quest for a vaccine to prevent polio went largely unanswered. It wasn’t until 1948 when Doctor Jonas Salk, working for the University of Pittsburgh was awarded a grant to study the polio virus and develop a possible vaccine when another serious attempt to eradicate the disease took shape.

Salk studied Maurice Brodie’s work from the 1930’s. Much like Brodie’s earlier work, Salk’s procedure involved killing strains of the virus and then injecting the benign viruses into a healthy subject’s bloodstream. The subject’s own immune system would then create antibodies that would resist future exposure to poliomyelitis. Salk conducted the first human trials on former polio patients, then upon himself, and finally his own family. After five years of research and initial testing, on March 25, 1953, he was ready to announce his findings. He did so on the CBS radio network. Two days later, his work was presented in an article published in the Journal of the American Medical Association. The world was finally optimistic about curing the disease that had altered so many children’s lives.
**********
Here at Home
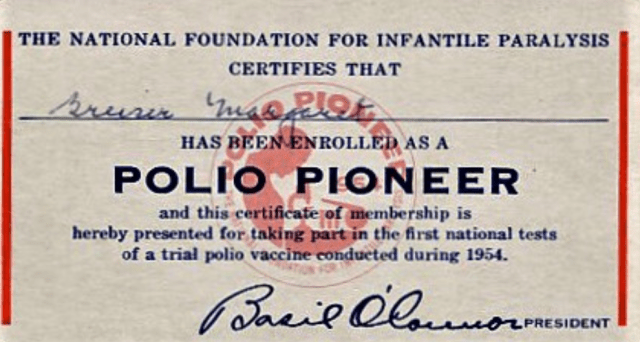
By early 1954, the most feared disease by many parents in Easton was likely infantile paralysis, more commonly known as polio. The disease had reached epidemic proportions in 1952 with a record 57,879 cases reported that resulted in 3,145 deaths. Nationwide, parents were frantic. In what virtually everyone in today’s world would consider unthinkable, parents desperate to save their children from the horrors of this deadly and incredibly debilitating disease offered up a total of 1.8 million of their offspring to serve as test subjects for the vaccine developed by Salk. A vaccine that promised to all but eradicate the illness. These children were boldly dubbed the Polio Pioneers.

The risk of contracting polio was highest during the summer, so getting the first children inoculated by the late spring of 1954 was imperative if there was to be any hope of proving the new vaccine effective enough to make it available nationwide by the following year. The Salk polio vaccine trials became the largest mobilization of volunteers in American peacetime history. Over 325,000 doctors, nurses, educators, and ordinary citizens pitched in. The only funding came from $7.5 million in donations given to the National Foundation for Infantile Paralysis. A good deal of those donations came from the annual Mother’s March that was more commonly referred to as the March of Dimes. No government monies, no big pharmaceutical companies; just donations from ordinary Americans united in their efforts to bring the horrors of polio to an end.
The test subjects were randomly divided into two groups. In one group, half of the children would simply be observed for signs of the disease, while the other half would receive the vaccine. In the second group, half would be inoculated with the new vaccine, while the other half received a placebo. The tests were “blind” so that neither the health practitioners, nor the patients, knew who received the vaccine and who didn’t. In 1954, there were no computers available for recording the inoculations, so it was all done by hand, and all by volunteers. In all, some 653,000 children received a total of three injections each, with 443,000 of them receiving the actual polio vaccine and the other 210,000 receiving the placebo.
The late summer and the entire autumn of 1954 were spent taking blood samples from over 40,000 of the vaccine’s recipients and waiting to judge the rate of success of the new drug. The final results were astounding, the Salk vaccine proved to be 80 to 90 percent effective in preventing polio! In early 1955, the New York Times ran with the headline, “SALK POLIO VACCINE PROVES SUCCESS; MILLIONS WILL BE IMMUNIZED SOON; CITY SCHOOLS BEGIN SHOTS APRIL 25.”
I was one of the first ordinary students in the spring of 1955 to receive the vaccine. We stood in line while the school nurse checked off our names and someone in a white lab coat rubbed the spot with alcohol where the injection would be administered before then stabbing us with a needle full of medicine. That injection very likely spared at least some us the pain and suffering of polio, a disease that within ten years of Jonas Salk’s amazing work would be virtually wiped out. In 1955, due in large part to the Salk vaccine, polio cases in the United States dropped to 13,850 and deaths to 1,043; a 66% decline in mortalities in just 24 months. As I look back at the remarkable events of 1954, I can only offer my sincerest thanks to those who became known as the Polio Pioneers.
It should be noted that the Salk vaccine immunization campaign almost came to a very unfortunate end in 1955 when in April of that year, more than 200,000 children in five Western states received a polio vaccine in which the process of inactivating the live virus proved to be defective. Within days there were reports of paralysis. The first mass vaccination against polio was temporarily halted on the 8th of May. Subsequent investigations revealed that the vaccine, manufactured by the California’s Cutter Laboratories, had either caused or failed to prevent thousands of new cases of polio, leaving 200 children with some degree of paralysis and killing 11. There were five laboratories licensed to produce the Salk vaccine and when only the Cutter vaccines were found to be defective, the mass vaccination process was allowed to continue.

A very special thanks goes out to Margaret Greiser Perry, a Polio Pioneer who received her card during that crucial time of testing at the Samuel Staples School, and who has very graciously shared it with the Historical Society of Easton. It’s folks like Meg who saved many others!

